Q&A: What It’s Really Like to Manage Multiple Chronic Conditions
An interview with Sam Anderson, founder of Invisible Illness Living
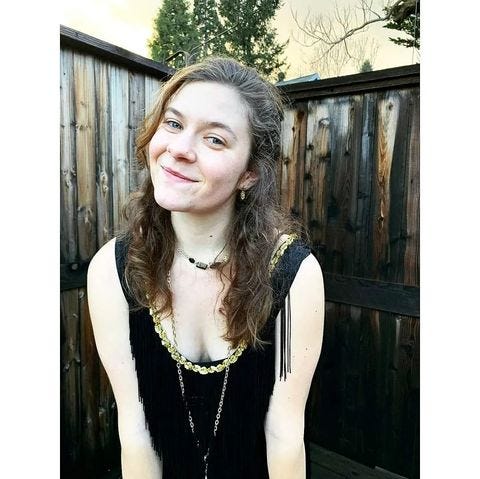
I recently met Sam Anderson through my volunteer work at Beyond Celiac. She’s a fellow ambassador for the organization and the founder of Invisible Illness Living. I’ve really enjoyed Sam’s content on Instagram about living with multiple chronic illnesses (including celiac disease, POTS, PCOS, and IBS).
She does a fantastic job providing educational information about these various illnesses and showing what it’s really like to navigate life with multiple chronic conditions. She also shares her favorite gluten-free eats in Portland, Oregon (one of the best cities in the US for gluten-free food).
I knew I had to feature Sam in my newsletter and I was thrilled when she sat down with me for an interview a few weeks ago. Ahead, Sam shares her path to celiac diagnosis, how she handles managing multiple chronic health conditions, and what inspired her to start her website and Instagram account.
If you’re not already following Sam on Instagram, I highly recommend you do so! She also has a podcast called Chronically Yours and two invisible illness journals available for purchase (here’s Vol. 1 and Vol. 2).
Q: Tell me about your path to celiac diagnosis.
A: Growing up, I never liked the taste of bread or gluten-y things. I thought they tasted bad, and my parents just thought, “Oh, my kid doesn’t want to eat a sandwich or pasta.”
I would even schedule play dates so I wouldn’t be at one specific friend’s house because her dad brought home donuts on Sunday mornings and I hated donuts.
That was the extent of it until I was in college. I thought bread was gross. Pretzels were weird. I just didn’t want any of it. Luckily, my parents were totally happy to follow what I wanted to eat.
And then in college, when I was 18 during the first winter break home, I had sinus surgery and woke up with celiac symptoms. Before then, we didn’t think anything about it. I never got sick.
But about three weeks after that surgery, I was back in college and my roommates and I ordered pizza. I ate a slice and a half and then bolted up. I was in the bathroom the whole night.
I thought to myself, “Oh my God, what is happening to me?” I had a low bed, and I remember the next morning, I couldn’t stand up because my stomach was so swollen.
I rolled out of bed and sort of pushed myself up onto the floor. When I looked in the mirror, I was like, “Wow, I look pregnant.” I had never seen my body look like that.
I wore baggy clothes for a week and thought maybe I had gotten food poisoning. But I kept getting more sick and stayed in the bathroom for hours.
I experienced swelling, stabbing, diarrhea, and none of my clothes fit. I was really nauseous all the time, but I never threw up. It was basically just a constant state of, “Am I going to puke?”
For about a week, I couldn’t eat anything. I was drinking a bunch of water and that’s it. At the end of that week, I was on a call with my friend who had stayed an extra week visiting somebody for Christmas break, so she wasn’t home yet.
I was telling her all of my symptoms, and she said, “Well, you sound like the friend that I’m staying with. She has celiac disease.” And I was like, “Huh. I can’t have a disease, but thanks.”
I dismissed it for a day, but then thought, “Well, maybe.” But it was that kind of struggle between, I was so healthy and then I was not. I thought, “I can’t be a sick person,” because I was healthy three weeks ago.
Until that surgery, everything was fine. And then I progressively kept getting sicker. Luckily, one of my best friends was studying biology, so I called her and asked, “Can you tell me what’s happening in my body? What should I do?”
She was giving me basic lessons about how the digestive system worked and gave me some things to Google. She’s the one who suggested I try an elimination diet.
I didn’t want to go to a doctor, so I took my friend’s suggestion and felt a bit better by the end of that. I was like, “Okay, something’s up with this whole gluten thing.”
I went to Google “what is gluten” and I saw this big list and thought, “I can’t do it.” I was kind of in this gray area where I took out the obvious things that contained gluten but didn’t do the research I should have. As an example, I was still eating normal soy sauce but knew not to eat a hamburger bun.
While all of these changes were happening, some fairly important people in my life died. Having to handle grief not only for my body but also for these people was way too much, so I dropped out of college.
My actual celiac diagnosis period was fairly quick. I saw my first primary care doctor at the beginning of September and was diagnosed at the end of October.
The first doctor I saw was like, “You’re 19. Lose some weight and drink some water.” And I said, “No, can I at least have a blood test?”
He told me that it was expensive and a waste of my time. I said I didn’t care if it was expensive, I wanted it. He responded, “You just need to settle yourself.” It made me so angry.
I demanded to have this test. I said, “I don’t care if it costs money.” He reluctantly did the test and it was confirmed as positive for celiac disease. His response was, “False positives happen all the time,” which isn’t true.
I was again in this position where he didn’t want to help me. I needed to see a gastroenterologist. I had been doing enough research where I knew the steps.
I told him I wasn’t leaving until he gave me a referral. I even stood up in the office, which probably wasn’t the best idea, but it got me there. It’s tough when you’re young sometimes to be taken seriously.
I got into the GI really quickly. There was a cancellation, so it was crazy fast. I went in and explained my symptoms and the GI was like, “Whoa, sorry about your primary care. Let’s get you into testing now.”
It was only about a week or two later that I had the endoscopy. He was very concerned and very shocked because he said my villi were supposed to look like shag carpet but they looked like college dorm room carpet.
So, I had my diagnosis of celiac and he also handed me a packet for GERD (gastrointestinal reflux disease) and some general IBS paperwork and sent me on my way.
That was it. There was no help after that. It was just like, “Okay, here’s your packet of the diseases you have. We’ll check back in a couple of months and see if you’ve done a good job.”
Q: How did you handle the switch to going gluten-free?
A: Honestly, it wasn’t very hard because at that point, the only things I could stomach were bone broth and garbanzo beans. When I moved home from college, my parents and I had assumed it was celiac disease. They had done a lot more research than me because I was still in the mindset of, “I’ve got to succeed in college. My body can handle itself later.”
My parents are divorced and both of them decided to remove gluten from their houses when I moved home from college. I was both very thankful and incredibly guilty. I was like, “This is expensive and time-consuming.”
They had to change their lives. At the same time, I was thankful that this was an option because now I had two places that were very safe for me.
I dropped 20 pounds in two weeks, which was right about the time I got the endoscopy. I was just failing. After a couple of months, by December, I was eating more solid food again.
I could handle some vegetables, fruits, and rice. It wasn’t too hard to go gluten-free, I think, because everything with gluten had been taken out of the house and we were bringing in new things.
I didn’t have to worry about trying to figure out what was going to hurt me in the house. It was, “What are the things that I would like to try to eat,” and then looking at them before going to the store, figuring out what the options are, and then bringing them home.
Q: Were there any siblings at home with you?
A: So, I’m an only child with divorced parents. It was fine because it was just me having to be the problem. When I moved home, I moved in with my dad and he honestly kept me alive. I was so incredibly sick. I lost a lot of weight. I couldn’t walk across the room. I couldn’t even open a water bottle.
I slept on the couch, and my dad brought me food. I watched Friends and I slept a lot. It was really tough for both of my parents to see me like this. They were very scared, but I wouldn’t let them come with me to doctor’s appointments.
I think it would’ve made things easier if I had let them come with me. But I felt like there were so many things being taken from me that driving myself and going alone was one of the only things that I could keep that autonomy over and be able to feel like a human being.
Q: You mentioned that you started eating solid food again a couple of months after your celiac diagnosis. Was there a point where you started feeling “better” health-wise after that?
A: Not really, but I came up with a benchmark: As soon as I could hold my camera again for one hour without having to sit down, I assumed I would be well enough to care for myself. I don’t know where I came up with that idea, but that’s what happened.
In mid-January, I hit that goal where I could hold my camera. I didn’t feel well, but I was at least maintaining weight. I could walk around and drive myself without stopping to go to the bathroom.
I moved to Oregon at the end of February because that seemed like a good idea. Honestly, it was the best idea for me and it’s still the best place for me to be. But looking back, it was too fast.
I tried to go to school in Oregon, thinking I was “better.” I moved up to Portland and was in one of the small towns about 10 minutes outside the city.
I was working with kids as a nanny when I realized I was not better and I ended up having to drop out of that program as well and then move back in with my dad again. This time I didn’t have to sleep on the couch at least.
All of my 20s, I’ve been a patient and have not been able to hold an actual job. I’m always trying all kinds of different ways to figure out how to make a business and figure out how I fit into the world, but it’s really difficult with how many different issues I have.
It’s not just my gut. I have some sort of condition for almost every part of me. POTS, now I don’t have eardrums anymore, so I have hearing aids. PCOS. There are just so many different pieces that I always have something going on.
I recently moved back up to Oregon for the third time, and since moving here in August, I’ve had a doctor’s appointment every day, Monday through Friday.
There are a couple of blank days peppered in here and there, but not many. Oftentimes, there are two doctor’s appointments a day and then there’s testing, calling insurance, calling doctors, having to talk with other specialists, and updating primary care.
Picking up medications, going to physical therapy, and making sure I exercise enough to help the issues of one set of symptoms without over-exercising and causing flares for another set. There's so much to managing all of this that I don’t know if I have time for anything else.
Being on a gluten-free diet saved my life, but it didn’t necessarily make it “better.” I don’t know if I would use the word better. I think I’m healthier than when I was first diagnosed, but I can’t use the word better.
Q: How long ago was your celiac diagnosis? And when did you receive some of your other diagnoses?
A: We’re coming up on 10 years for my celiac diagnosis. To give some context to my other diagnoses, back when I was 17, I got a concussion and it was really bad. I was out of school for three weeks. I had to cut my hair because it was too heavy and gave me migraines, and I lost the ability to recognize people’s facial expressions.
I couldn’t figure out if somebody was angry with me or happy. It completely set me back and resurfaced all of the learning issues I had as a child. I couldn’t read out loud, I couldn’t count. I couldn’t read the clock face. That had a lot to do with why college was such a struggle and why I had to drop out. My brain was still healing.
After the concussion, I started experiencing what we now know are POTS and vasovagal syncope symptoms, where when I stand up, I get really dizzy and pass out in certain circumstances. I can’t regulate my nervous system very well.
The vasovagal syncope diagnosis happened around the same time as my celiac diagnosis. So it was celiac disease, GERD, IBS, vasovagal syncope, and oral allergy syndrome.
I went to an allergist who did one of those scratch tests and he was like, “You’re intolerant to food. You know how to manage your body so good luck.” That was all before I turned 20.
PCOS and POTS came later. I had to have some corrections done from the sinus surgery I had when I was in college, and because of those corrections, my eardrums disintegrated and I developed tinnitus and hearing loss. I have very big holes in my eardrums. I was also diagnosed with fibromyalgia. That gives you an idea—most of my body has something.
Q: What advice do you have for someone who has celiac disease and other chronic conditions?
A: What I like to do is break my body down into categories. It makes it a lot easier to at least visualize what’s happening if I can group things into categories. That way I can try to map what flares come from what category and how they cross over.
There’s going be some things that blend together, like with PCOS and IBS. I miss my periods a lot. I’ll sometimes go three months without one. But within those missed periods I will get really constipated, and I’ve been told that is probably because some sort of hormonal fluctuation is happening but not enough for me to actually have a period.
So they’re all kind of looped together and twisted in on each other. If you can find a way to separate them into categories but learn where the crossover is, then I feel like that can help.
It gives you something to think about, like, “Why am I constipated? Is it because I ate something or is it because there’s a hormonal fluctuation happening?”
Another tip is to take things slow. Slow down your life as much as you possibly can because it’s a lot to manage. It’s very difficult. It can be very isolating and it’s often exhausting. So if you can try to slow it down to give yourself enough space and time to learn your body, that’s ideal.
That’s what I did for the first five or so years. I hardly used technology. I had a little house and a little garden and a dog. I slowed down, put my hands on some dirt, and grew some vegetables.
I was lucky enough to make some friends post-diagnosis who were willing to support me, and we played a lot of Dungeons & Dragons. It’s all about finding what works for you and relearning how to live.

Q: When did you decide to launch your website and Instagram account, and why did you get started?
A: It’ll be two years in July, so not very long ago. Part of that is because when I was first diagnosed, I did try to be part of communities, and honestly, it was too hard. People were too mean.
At the beginning, I thought, “Maybe I can meet some other people who are young and have celiac disease.” Then I tried posting a couple of questions on forums and Facebook pages and I was getting eaten alive. I was done. So that’s part of why I wanted to start my own account.
There have been so many people I’ve met through this that I’ve been able to collaborate with and do things with that I never would have if I hadn’t started that page.
I have a podcast now. It’s so much fun, but I’m glad I’m co-hosting it because it’s so much work. But it’s also really neat. It’s not something I would’ve ever thought to do before.
Q: What types of content do you share on Instagram?
A: People keep telling me I need to choose a niche, but it’s too hard. The reason I chose my name, Invisible Illness Living, is because I wanted to give myself the freedom to talk about whatever is being a problem at that moment. And I do that a lot. I don’t follow a strict rule. I like to talk about what’s happening to me. I tend to do reels.
I like to talk about the doctor’s appointments I go to. I most recently started doing more of those videos where I’m explaining what doctor’s appointment I’m going into or going out of. Or, I’m talking about symptoms or taking a certain medication.
My hope and point to all of this is to connect with two kinds of people: Either people who are going through something similar and don’t want to feel alone or people who are support systems and don’t know what’s happening to their loved ones.
Because it’s chronic illness, and autoimmune, there’s most likely going to be two or three (if not more) conditions that are happening simultaneously.
I’m really trying to be honest about what my body’s doing and what my day-to-day looks like. I’m trying to show people what’s going on and hope that others can learn from it or can laugh with me or cry with me or be angry with me because it’s our real life.
Q: What else would you like to tell someone who has celiac disease and/or multiple other chronic conditions?
A: With celiac disease, remember that you're probably not going to feel better immediately. Some people may, but it usually takes six months to a year for the healing to actually happen.
Along with that, if you don’t feel better, keep pushing. I don’t know that I’m ever going to feel like I did before my diagnosis. And this whole thing, like, “the gluten-free diet is going to make you feel like a normal person,” that’s never been the case for me at all. It stumps and frustrates doctors a lot.
But the takeaway from that, that I want other people to know, is if you feel like something else is wrong with you, then you are totally within your rights to push for that. Do the tests, talk to the doctors, see if there’s a sub-specialist or maybe get a second opinion.
Do whatever you can because the more you understand about your body, the easier it’s going to be to find that strength and also to manage what’s happening to you.
A lot of it we can’t control, but you can do your best to name the issues. I find that if I have a name for something, then it doesn’t make it better but it does make it easier to categorize.
I’ll add one more piece of advice about meeting new people when you have celiac disease. It can be very overwhelming for people who are new to you to hear all of the things that have to happen in order to make you safe. What I’ve found is making a priority list and slowly introducing new people to these concepts helps.
If I’m meeting a new group of friends, I’m going to eat beforehand and I’ll show up with a bag of tortilla chips or something like that because I want to be nice. But I try to explain things in smaller doses so that it’s easier for people to understand.
When you have multiple conditions, prioritize the ones that are going to be most detrimental if something happens. And then, as I get to know people, I add in another one. But there’s no reason to list everything all at once.
Like with celiac disease, it’s the first thing I talk about with anybody—I even put it on my dating profiles. It’s out there. Everyone knows I don’t eat gluten and that I don’t touch it.
Just because we have invisible illnesses, doesn’t mean we deserve to have less. So be patient and take the time to learn about yourself. Find what you like, find what works for you, and find people who will support you. Your life may look different, and that’s okay.
Photos courtesy of Sam Anderson
Disclaimer: If you click on a link, I may get a small commission. This helps support this newsletter so I can keep writing it.







This was a really good interview. It is so important to bring the challenges of invisible illnesses to light, in the healthcare system, in personal relationships, and of course the internal grief and adjustments. Bravo.